Home > African Marke > Tanzania
Time: Jun 17, 2016
AIDS Epidemic and Response
AIDS epidemic in the country
Number of people living with HIV | 1,500,000 [1,300,000 - 1,900,000] |
Adults aged 15 to 49 prevalence rate | 5.3% [4.8% - 5.9%] |
Adults aged 15 and up living with HIV | 1,400,000 [1,200,000 - 1,800,000] |
Women aged 15 and up living with HIV | 800,000 [710,000 - 1,200,000] |
Children aged 0 to 14 living with HIV | N/A |
Deaths due to AIDS | 46,000 [36,000 - 80,000] |
Orphans due to AIDS aged 0 to 17 | [550,000 - 1,800,000] |
Source: HIV and AIDS estimates (2014)[1] from UNAIDS Data
General description: during the period 2003/42 to 2011/123, the HIV prevalence in Tanzania has declined from 7.0% to 5.3% among adults aged 15-49. Statistically significant decline was observed among men in the same age group from 6.3% to 3.9% but not among women. Data from four rounds of antenatal surveillance, two national population surveys and projections indicate that HIV incidence in the age group 15-49 peaked at 1.48% in 1991, declined to 0.6% in 2004 and stabilized at 0.59% up to 2011.
This decline in HIV incidence partly explains the observed decline in HIV prevalence. Despite the decline, the HIV epidemic in Tanzania remain heterogeneous with geographical and population variability. The HIV prevalence ranges from 1.5% in Manyara to a high of 14.8% in Njombe. While HIV prevalence is generally at decrease, 8 regions namely Ruvuma, Kagera, Kigoma, Rukwa, Mtwara, Kilimanjaro, Singida and Arusha have recorded an increase. It is not clear so far as to what is the cause of the increase but could be due to increased HIV incidence or impact of scaling up care and treatment in these regions.
HIV infection among young people aged 14-25 is an important proxy indicator for determining trend in HIV incidence and prevalence. The overall change in HIV prevalence among young people aged 15-24 from 2007/08 (2.4%) to 2011/12 (2.0%) is equivalent to 17% decrease during the past 5 years. In comparison to three HIV indicator survey there is decline of HIV prevalence among youths aged 15 -19 for both girls and boys.
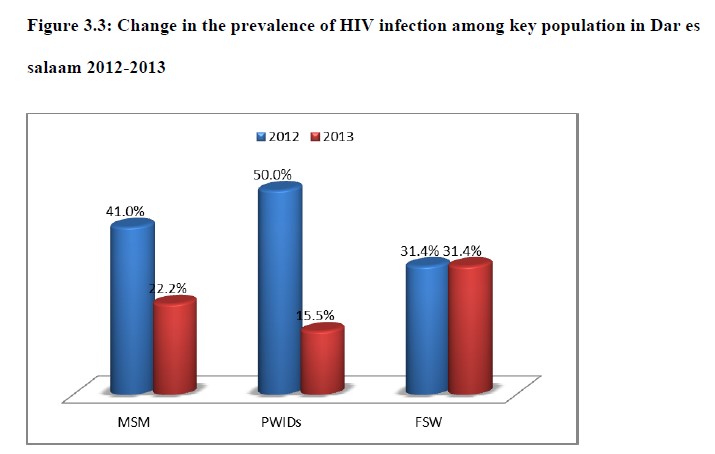
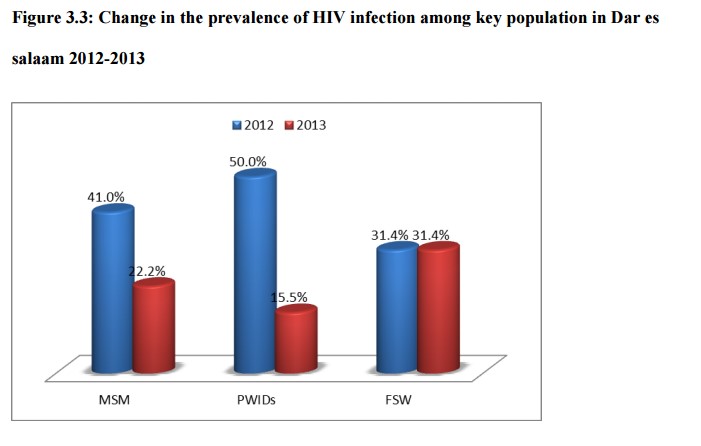
AIDS epidemic among key populations: HIV prevalence’s among key populations have been reported to be high. Available data from recent studies gives the prevalence of HIV among people who inject drugs (PWIDS) to be 16%, Men who have sex with men (MSM) to be 22.2% and Female Sex Workers (31.4%). Although these may not be national representative estimates, they show a decline in HIV infection among key population when compared to earlier estimates among MSM (42%) and PWIDS (51%).
Declining HIV infection rates in the general population and possibly among key population could be an indication of the impact of extensive preventive intervention measures in the country. The government of Tanzania collaborates with partners in the development and scaling up of evidence-based intervention measures aiming at reducing the rate of HIV infection.
National AIDS response
Tanzania has adopted an integrated strategy for the implementation of the prioritized HIV prevention Interventions. Prevention of new HIV infections remains the national priority in the fight against HIV and AIDS. Among the aims of NMSF III 2013/14-2017/18 are reductions or prevention of new infections if exposure has occurred, reduction of the probability of infection if transmission has occurred and finally influence behaviour change where social or cultural norms, values and practices remain barriers to adopting effective prevention behaviours.
Key populations: Based on few available studies from mainland Tanzania and Zanzibar, the HIV prevalence among PWIDS decreased from 50% to 15.5% by 2013. This decline was also noted among men who have sex with men with a decrease from 41% to 22.2%.
Maternal health & PMTCT: The country has adopted a virtual elimination of MTCT strategy with four prongs which are to reduce HIV incidence among women, increase access to Family Planning (FP) among women, reduce vertical transmission to <5%, and maternal and child mortality by 90% by 2015. To improve efficiency in health services delivery, integration of PMTCT services in the routine RCH services has been implemented with a remarkable 93% integration. A significant proportion (85%) of pregnant women is tested for HIV during ANC visits. HIV testing facilities have increased to 2137 with the integration of prevention of mother to child transmission (PMTCT) services into Reproductive and Child Health (RCH) facilities has reached 96% of facilities. But currently, 77% of HIV positive pregnant women are receiving Antiretroviral Therapy (ART) and the national goal is to reach 90% by 2017.
ARV: The number of people receiving ARV has been increasing steadily since 2010 and by December 2013, a total of 1,366,402 were enrolled in care and treatment centres, 512,555 PLHIV were receiving ARV of whom 8% were children.
Challenges and actions
1) There is lack of adequate human resource to carryout M&E activities at all levels, specifically at sub national levels. Many community HIV/AIDS committee members have not been trained on TOMSHA reporting and there is frequent change of TOMSHA officers. Supportive supervision is also not optimal due to lack of lack of supervision plans in most council;
2) Data emanating from lower level reporting have been of poor quality due to poor documentation on implemented HIV and AIDS activities by various civil society organizations (CSO). Data management at service delivery points have not been carried out in a systematic manner. This has been cemented by the inadequate capacity on management of TOMSHA electronic database by most of the Councils HIV Coordinators. Non-medical HIV programs have not been reporting regularly as required resulting in problems in tracking programme implementation and coverage;
3) Systematic collection and reporting of data on key population has not been possible. Routine collected data are not disaggregated by population characteristic to be able to identify key population. This limits tracking service access among key population.
[1] http://www.unaids.org/en/regionscountries/countries/unitedrepublicoftanzania/

