Home > African Marke > Ghana
Time: Jun 17, 2016
AIDS Epidemic and Response
AIDS epidemic in the country
Number of people living with HIV | 250,000 [190,000 - 330,000] |
Adults aged 15 to 49 prevalence rate | 1.5% [1.1% - 2.0%] |
Adults aged 15 and up living with HIV | 230,000 [180,000 - 300,000] |
Women aged 15 and up living with HIV | 140,000 [110,000 - 180,000] |
Children aged 0 to 14 living with HIV | 21,000 [16,000 - 28,000] |
Deaths due to AIDS | 9,200 [7,000 - 13,000] |
Orphans due to AIDS aged 0 to 17 | 120,000 [85,000 - 250,000] |
Source: HIV and AIDS estimates (2014)[2] from UNAIDS Data
General description: The number of new HIV infections has reduced from 13,272 in 2011 to 11,356 in 2014; adults contributed 83% and children 17% of new HIV infections in 2014 and young people 15-24 years of age contributed 26% of new HIV infections in 2014.
The estimated number of mothers in need of Prevention of Mother to Child Transmission of HIV (eMTCT) reduced from 10,869 in 2011 10,226 in 2014. PMTCT coverage has increased from 74.1% in 2011 to 81.2% in 2014. The estimated final transmission rate has reduced from 20.3% in 2011 to 18.5% in 2014.
In 2014 the highest prevalence was in the 30–39 year age group (3.2%) followed by the 30–34 year age group (2.8%), and the least prevalence of 0.9% was in the 15-19 year age group.
In 2013 the overall mean and median prevalence in urban areas exceeded the rural prevalence (2.2% versus 1.3%). There were increases in prevalence all regions but the Central, Eastern, and the Brong-Ahafo regions.
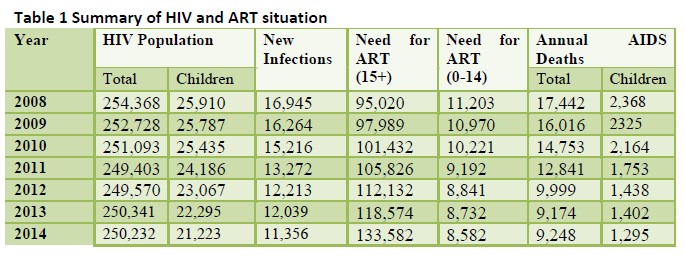
The estimated number of patients needing Antiretroviral Therapy (ART) also increased from 127,306 in 2013 to 142,164 in 2014. Of these 8,732 and 8,582 respectively were children. It is estimated that of the 133,582 adults needing ART in 2014, 49,267 are males and 84,315 are females.
AIDS epidemic among key populations: HIV prevalence in Key Populations (KPs) has been consistently higher than the general population. In 2009, the HIV prevalence among sex workers was 25.1% which is a decline from the 34% in 2006. (The modes of transmission study have indicated that low risk heterosexual sexual activity (30.2%), Casual heterosexual sex, (15.5%) and sex with partners of clients of sex workers (23.0%) contributed to most of HIV incidence in 2008). The recent studies (The Men’s study and the IBBS, 2011) in key affected populations show that prevalence among FSW is 11.1% overall and for MSM 17.5%.
National AIDS response
Key populations: FSWs, MSM, prisoners, and PWIDs are identified in the NSP as key drivers of the epidemic. A complementary Key Populations Strategy 2012-15 was developed to reach at least 80% of identified KPs with HIV prevention information and services. Funding for the KPs interventions was provided by PEPFAR Global Fund, and the GoG. HIV prevention information and services were provided for FSWs, MSM, and prisoners but not for PWIDs during the period under review. Key activities implemented during the review period to reach about 50,000 - 60,000 KPs (FSWs and MSM) include targeted behaviour change communication and interventions through provision of HIV prevention information and services (psychosocial support, HTC, diagnosis treatment for STIs, condom and lubricant promotion and distribution, and appropriate referrals). In 2014, GAC collaborated with the University of Cape Coast, and CDC to execute Formative Studies to assess the situation of drug use including Injecting Drug Users (IDUs) in Accra, Tema, Sekondi-Takoradi, Cape Coast and also with Kwame Nkrumah the University of Science and Technology, the Boston University and PEPAR in Kumasi to implement a study on HIV Vulnerability of Men and Women Who Inject Drugs in Kumasi. In addition SOPs were developed and M&E Officers together with project managers from selected CSOs were trained with support of FHI360 in 2014.
Elimination Mother to Child Transmission(eMTCT): An HIV prevalence of 1.6% (Confidence limits: 1.42-1.81) in pregnant women (HIV Sentinel Survey 2014) versus 1.47% in the general population in 2014 reflects the weakness in performance in implementing eMTCT prongs 1 and 2, although there has been improvement over 2012 and 2013 figures. The NSP has adopted elimination of mother to child transmission of HIV (eMTCT) as the preferred strategy to achieving overall reduction of new HIV infections in children. The main outcome is to reduce MTCT of HIV from 30% in 2010 to less than 5% by 2015. To achieve this outcome, Ghana committed to implementing all 4 prongs of the comprehensive eMTCT approach and rapidly scaled up its eMTCT program by increasing facilities providing services from 793 in 2009 to 863 in 2012. NACP data indicates that in 2013 69% of HIV infected pregnant women received ARVs prophylaxis to prevent mother to child transmission of HIV. This figure rose to 81.2% against the NSP target of 70% in 2014.
ART: Ghana has rapidly scaled up its ART program by increasing the number of ART sites from 79 in 2010 to 160 in 2012, 175 in 2013 and 179 in 2014, whiles training a significant number of ART service providers to provide quality services. The target number of patients has increased from a baseline of about 38,000 in 2010 to about 56,000 in 2011 and to about 97,494 in 2014. Nearly 100% of all patients targeted to receive ART services did receive treatment in both years, as adequate funding was available to meet the treatment cost for this group. A similar outcome was achieved for 90,756 patients of those that were eligible (83,712 clients) to receive treatment in 2014. However, based on total need for ART services only 49% of all patients eligible for ART in 2011 received the treatment, this figure increased to only 55% in 2012, and was 69% in 2013, primarily due to the inadequate funding for the ART program.
Challenges and actions
1) Prevention of Mother-to-Child Transmission (PMTCT): stock out of PMTCT commodities including RTKs, ARVs, and reagents from CD3 counts machines greatly retards progress towards reaching programme targets; the implementation of Prongs 1, 2, and 4 are weak; the coordination roles for Family Health Division (FHD) and NACP have not been well defined resulting in leadership-related challenges as both have mandates that cover the provision of services to pregnant women and to HIV infected mothers and their HIV exposed babies; full integration of SRH and HIV services has not been attained at some facilities and referrals still being done even within the same facility;
2) HIV testing and counselling (HTC): erratic HIV test kits supply for a considerable period during the period under review did not only compel the HIV programme to abandon the KYS campaign that contributed immensely to access to the HTC services, but also may contribute to people losing interest in HTC, as those who need services cannot get them;
3) Blood safety: lack of funds to embark on sustained blood donation campaigns as well as inability of centres to recruit and maintain VNRBD is a major challenge facing most of the blood transfusion centres especially in the rural areas; blood banks are almost always near empty and family members as well as paid donors unfortunately step in almost always to save the situation;
4) Post-exposure Prophylaxis (PEP): PEP, like PMTCT, is a top priority even in situations of low ARV availability; some professional staffs that have been exposed to the risk of HIV infection may be reluctant to report at ART centres for PEP;
5) Treatment: inadequacy of trained staff to manage patient is a major challenge; none or delayed reporting of data couple with high risk of data errors during transfer of data from primary source to the reporting forms characterized STI documentation; shortage and erratic supply of ARVs and CD4 count reagents which had characterized the ART program operations was less marked during the reporting period 2013 and 2014;
6) Care and support: the WFP food supplementation programme to food insecure households in the 3 northern regions and in the Eastern region is limited to only 600 patients and up to 4 dependents; food supplementation should continue to be administered alongside the ARVs at the clinics as efforts to move the food rations away from the ART sits are not in the interest of patients; the present guidelines which require PLHIV to be weaned off after six months of intervention once they have improved nutritional status (BMI > 18.5kg/m²) is difficult to be strictly adhered to and some beneficiaries are supported for a year or more.
[1] Ghana AIDS Commission, Country AIDS Response Progress Report - Ghana, March 2015, http://www.unaids.org/sites/default/files/country/documents/GHA_narrative_report_2015.pdf
[2] http://www.unaids.org/en/regionscountries/countries/ghana/

